Healthcare workers are vital to our society, providing essential medical care and services to patients. However, their work environment exposes them to numerous risks, one of the most significant being exposure to bloodborne pathogens. Bloodborne pathogens are infectious microorganisms present in blood and other body fluids that can cause serious diseases. Understanding the most common risks of exposure and implementing effective preventive measures are crucial for ensuring the safety and health of healthcare workers.
What Are Bloodborne Pathogens?
Bloodborne pathogens are microorganisms, primarily viruses and bacteria, that are transmitted through contact with infected blood or other potentially infectious materials. The most common bloodborne pathogens include:
- Hepatitis B Virus (HBV): This virus affects the liver and can lead to chronic liver disease, including cirrhosis and liver cancer. HBV is highly infectious and can survive outside the body for at least seven days.
- Hepatitis C Virus (HCV): Like HBV, HCV affects the liver and can cause chronic liver disease. It is a major cause of liver cirrhosis and cancer. HCV is primarily transmitted through blood-to-blood contact.
- Human Immunodeficiency Virus (HIV): HIV attacks the immune system and can lead to Acquired Immunodeficiency Syndrome (AIDS). It is transmitted through contact with infected blood, sexual contact, or from mother to child during childbirth or breastfeeding.
- Human T-Lymphotropic Virus (HTLV): HTLV can lead to conditions such as adult T-cell leukemia/lymphoma and tropical spastic paraparesis. It is less common but still a significant concern in some regions.
Common Risks of Exposure
Healthcare workers face several potential risks of exposure to bloodborne pathogens. Understanding these risks helps in developing effective preventive strategies and reducing the likelihood of infection. The most common risks include:
1. Needlestick Injuries
Needlestick injuries are one of the most common and significant risks for healthcare workers. These injuries occur when a needle or sharp object contaminated with blood or other infectious materials punctures the skin. Needlestick injuries can happen during various procedures, such as:
- Drawing blood samples
- Administering injections
- Handling needles after use
The risk of infection from needlestick injuries depends on several factors, including the type of pathogen, the amount of blood involved, and the worker’s immune status. For instance, needlestick injuries involving HBV are highly concerning due to the virus’s high infectivity rate.
2. Exposure to Blood and Other Body Fluids
Healthcare workers are frequently exposed to blood and other potentially infectious materials (OPIM), such as:
- Syringe contents
- Wound exudates
- Body fluids (e.g., vomit, urine, feces)
These exposures can occur during routine patient care activities, such as wound care, catheter insertion, or handling soiled linens. Proper handling and disposal of contaminated materials are crucial to minimizing the risk of infection.
3. Contact with Contaminated Surfaces and Equipment
Contaminated surfaces and medical equipment can also pose a risk of exposure to bloodborne pathogens. Pathogens can survive on surfaces and equipment for varying periods, depending on the environment and the pathogen. Common scenarios include:
- Handling used medical instruments
- Cleaning and disinfecting contaminated surfaces
- Touching surfaces contaminated with blood
Proper cleaning, disinfection, and sterilization procedures are essential to reducing the risk of pathogen transmission.
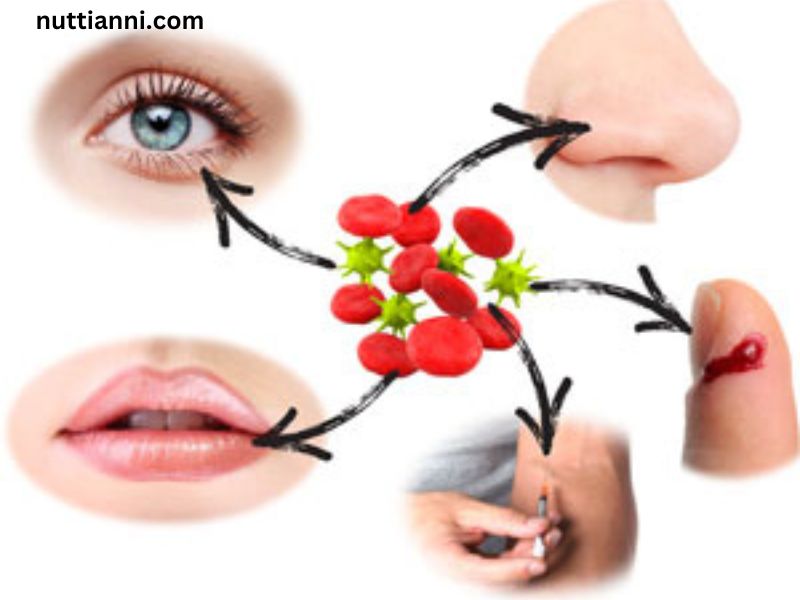
4. Splash and Spray Injuries
Splash and spray injuries occur when blood or other infectious fluids come into contact with the mucous membranes (eyes, nose, mouth) or non-intact skin (e.g., open wounds). This can happen during:
- Surgical procedures
- Emergency situations (e.g., trauma care)
- Laboratory work
Use of personal protective equipment (PPE), such as face shields and goggles, helps to protect against these types of exposures.
5. Improper Disposal of Sharps and Contaminated Waste
Improper disposal of sharps (e.g., needles, scalpels) and contaminated waste can lead to accidental injuries and exposures. Common issues include:
- Not using puncture-resistant containers for sharps disposal
- Improperly handling and disposing of contaminated materials
Adhering to established disposal protocols and using appropriate containers is vital to preventing accidents and exposures.
Preventive Measures and Best Practices
To protect healthcare workers from bloodborne pathogens, several preventive measures and best practices should be implemented:
1. Implementing Standard Precautions
Standard precautions are a set of guidelines designed to prevent the transmission of infectious agents. These precautions include:
- Hand hygiene: Regular hand washing with soap and water or using alcohol-based hand sanitizers.
- Use of PPE: Wearing gloves, gowns, masks, and eye protection as needed based on the procedure and potential exposure risk.
- Safe injection practices: Using sterile equipment and disposing of sharps in designated containers.
2. Providing Training and Education
Regular training and education for healthcare workers on bloodborne pathogen risks, safe practices, and emergency procedures are essential. Training should cover:
- Proper use and disposal of PPE
- Safe handling of needles and sharps
- Procedures for managing exposures and injuries
3. Implementing Engineering Controls
Engineering controls are designed to reduce the risk of exposure by modifying the work environment or equipment. Examples include:
- Needleless systems: Using devices that do not require needles to reduce the risk of needlestick injuries.
- Safety-engineered devices: Employing needles with built-in safety features to minimize exposure risks.
4. Promoting Safe Work Practices
Safe work practices help reduce the risk of exposure and include:
- Avoiding recapping of needles by hand: Using safety devices or one-handed techniques if recapping is necessary.
- Proper disposal of contaminated materials: Following protocols for disposing of sharps and other contaminated waste.
5. Post-Exposure Management
In the event of an exposure incident, immediate action is crucial:
- Wash the affected area: Rinse the area with soap and water or an appropriate disinfectant.
- Report the incident: Notify a supervisor and seek medical evaluation promptly.
- Follow-up care: Undergo testing and follow the recommended post-exposure prophylaxis (PEP) if applicable.
Conclusion
Exposure to bloodborne pathogens poses a significant risk to healthcare workers, with needlestick injuries, contact with contaminated surfaces, and splash injuries being the most common risks. Implementing standard precautions, providing adequate training, and using engineering controls are critical in minimizing these risks. By adopting these preventive measures, healthcare facilities can enhance the safety and well-being of their workforce, ensuring that healthcare workers can continue to provide essential care while minimizing their exposure to potential hazards.